Understanding Cancer: What We Know About Breast Cancer
ID
HNFE-980P
EXPERT REVIEWED
Did you know?
About 1 in 8 women will find out they have breast cancer at some point in their life (National Cancer Institute 2021a). Except for skin cancer, breast cancer is the most common cancer among women in the U.S., accounting for nearly 29% of newly diagnosed cancers. One case of breast cancer is diagnosed every two minutes, and one woman dies of breast cancer every 13 minutes in the U.S. (American Cancer Society 2021b).
Breast cancer is also the second leading cause of cancer death among American women, and the leading cause of cancer death among women ages 40 to 59. Although breast cancer in men is rare, an estimated 2,650 men will be diagnosed with breast cancer and approximately 530 will die each year. Death rates for breast cancer have steadily decreased in women since 1999 (fig. 1) as a result of improvements in early detection and treatment (American Cancer Society 2021b).

Breast Cancer Statistics
(American Cancer Society 2021b; National Cancer Institute Surveillance, Epidemiology, and End Results Program, n.d.)
About 1 in 8 women will find out they have breast Rates for new female breast cancer cases have been rising on average 0.3% each year between 2009–2018. In contrast, age-adjusted death rates have been falling on average 1.4% each year over the same time period
Estimated number of new cases of female breast cancer in 2021:
- U.S. cases: 284,200*
- % of all new cancer cases: 15%
*Estimated number of new cases of male breast cancer in the U.S. in 2021 is 2,650.
Estimated number of deaths of female breast cancer in 2021:
- U.S. deaths: 43,600*
- % of all cancer deaths: 7.2%
*Estimated number of deaths from male breast cancer in the U.S. in 2021 is 530.
Five-year Relative Survival Rate

The five-year relative survival rate for women with breast cancer depends on the stage at which it is diagnosed. Women with breast cancer found at the localized stage have a five-year survival rate of 90%. If the cancer has spread to nearby tissues or lymph nodes (regional stage), the survival rate is 84%, and if it has spread to distant organs (distant stage), the survival rate falls to just 26% (American Cancer Society 2019b). By following the breast cancer screening guidelines, women are more likely to discover breast cancer at an early stage when it is more treatable.
Types of Female Breast Cancer
(American Cancer Society 2021b and 2019c)
Most breast cancers are adenocarcinomas, which are cancers that start in the epithelial cells lining the milk ducts or the milk-producing glands (lobules). They can be described according to whether they have spread or not. In situ breast cancers have not spread, and invasive cancers have spread. The most common types include the following:
- Ductal carcinoma in situ (DCIS): DCIS is a non- invasive or pre-invasive breast cancer that develops in the milk duct. DCIS was estimated to make up 17.5% of new breast cancer cases in 2021.
- Invasive ductal carcinoma (IDC): The most common type of breast cancer, IDC starts in the cells lining the milk duct and has spread through the wall of the duct to nearby breast tissue. IDC makes up 70- 80% of all breast cancers.
- Invasive lobular carcinoma (ILC): ILC starts in the milk-producing glands, or lobules, and has spread to surrounding breast tissue. It can spread to other parts of the body and may be harder to detect than IDC. Just 1% to 3% of all breast cancers are ILC.
There are also less-common types of invasive breast cancers that account for less than 1 percent of all types of breast cancers.
Early Detection and Screening
(U.S. Preventive Services Task Force Guidelines 2016)
Breast cancer has several symptoms. Although all could be caused by other things, the American Cancer Society recommends that anyone experiencing the symptoms in table 1 should see a health care provider who is experienced in diagnosing breast diseases.
| Symptoms |
|---|
| Breast lump or mass |
| Breast Pain |
| Skin irritation/redness |
| Swelling of all or part of breast |
| Skin/nipple scaliness, redness or thickening |
| Nipple discharge |
| Nipple retraction |
| Skin dimpling |
Several types of imaging tests can be used to look for and diagnose breast cancer. The mammogram is a low-dose X-ray that is used to screen women for breast cancer. Two other tests are the breast ultrasound and magnetic resonance imaging (MRI). Breast ultrasound uses sound waves to create an image of the inside of the breast. An ultrasound is often used to look at breast changes felt on physical exam or to look at a suspicious area seen on a screening mammogram. Breast MRI uses radio waves and magnets to create detailed images of the inside of the breast. It is not recommended as a screening test for breast cancer, but it can be used in conjunction with a screening mammogram in women at high risk for breast cancer, and to gauge size and location of tumors in women with breast cancer.
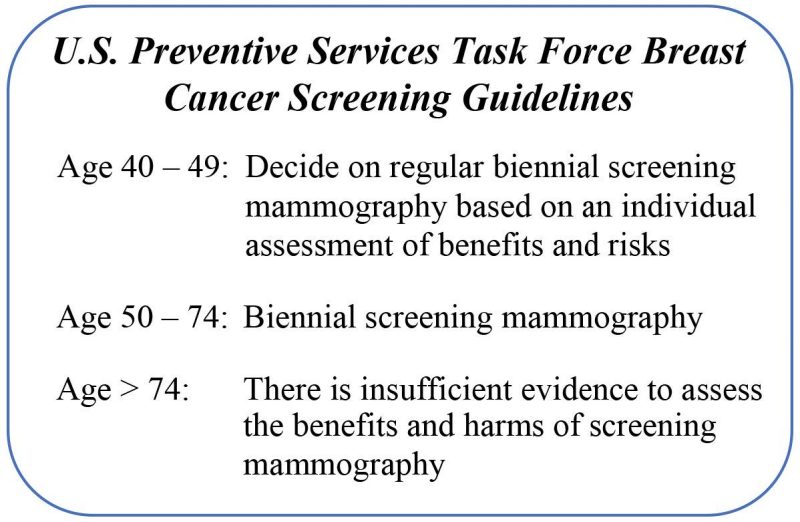
The U.S. Preventive Services Task Force issues guidelines on how often a woman should have a mammogram (fig. 3). Other organizations, including the National Comprehensive Cancer Network (NCCN 2021) and the American Cancer Society (2021a, n.d.a), have different screening recommendations. Decisions about when to begin screening for breast cancer should be made in consultation with a doctor and considering individual risk factors.
Treatment
(American Cancer Society, n.d.b; National Cancer Institute 2021b)
There are several treatment options for breast cancer. Treatment options are specific to the type and stage of the cancer and may consist of one or more local and systemic treatments.
Local Treatments
- Surgery: Most women with breast cancer have some type of surgery. There are two main types of surgery:
- Breast Conserving Surgery (BCS): Only that part of the breast containing the cancer is removed, along with some surrounding normal tissue.
- Mastectomy (removal of the breast): All of the breast tissue is removed.
- Surgery may also be performed to remove lymph nodes near the breast. Breast reconstruction surgery can be performed and should be planned with the surgeon early in treatment.
- Radiation: Radiation therapy consists of high energy rays that destroy cancer cells. Some women will need radiation treatment in addition to other types of breast cancer treatment. There are two main types of radiation therapy:
- External beam radiation therapy (EBRT): This is the most common type of radiation therapy. A machine outside of the body focuses radiation on the area affected by the cancer.
- Brachytherapy: Also known as internal radiation therapy, the radiation is delivered through a device containing radioactive pellets that is placed into the breast tissue for a short time in the area where the cancer had been removed
Systemic Treatments
- Chemotherapy: With chemotherapy, anti-cancer drugs are given intravenously or by mouth and travel through the blood to reach cancer cells in most parts of the body.
- Hormone therapy: These drugs stop cancer-promoting hormones, estrogen and progesterone, from attaching to hormone receptors on the cancer cells. It is recommended for women with cancers that are hormone receptor-positive, about 2 out of every 3 breast cancers.
- Targeted drug therapy: Anti-cancer drugs travel through the blood to all parts of the body, targeting specific unique changes in cancer cells.
- Immunotherapy: Drugs are used to stimulate a person’s own immune system to recognize and destroy cancer cells more effectively.
Risk Factors
The factors in table 2 are associated with increased risk of breast cancer.
| Risk Factors |
|---|
| Older Age |
| Being white |
| Obesity |
| Starting menstruation before age 12 |
| Menopause after age 55 |
| First pregnancy after age 30 or never having given birth |
| Post-menopausal estrogen and progestin hormone therapy |
| Recent oral contraceptive use |
| Radiation therapy to the breast/chest |
| Dense breasts |
High Risk Populations
(U.S. Preventive Services Task Force Guidelines, 2016 American Cancer Society 2021b)
Certain groups of people with similar characteristics are also at increased risk for developing breast cancer. These include people with:
A personal history of breast cancer (DCIS, IDC, ILC).
A family history of breast cancer in a first degree relative (mother, sister, daughter).
Genetic mutation (BRCA1, BRCA2, others).
Presence of certain benign breast conditions (proliferative lesions with and without atypia, lobular carcinoma in situ).
Note: Women with a high risk for breast cancer should start regular screening earlier. Consult a doctor about individual risk and screening recommendations.
Prevention
Anything that decreases the chance of getting a disease is called a protective factor. According to the National Cancer Institute (2014) and American Cancer Society (n.d.), the following recommendations are protective factors for breast cancer.
Know Your Risk
Talk to your doctor to determine if you have increased risk of breast cancer and whether you should have early screening.
Maintain a Healthy Body Weight
Gaining weight as an adult and being overweight or obese after menopause increases the risk of breast cancer. This may be due to estrogen production from fat tissue in post-menopausal women and increased insulin in women who are overweight (Key et al. 2011; Eliassen et al. 2006).
Eat a Healthy Diet
Choose foods and beverages in amounts that help maintain a healthy weight, limit consumption of processed meat and red meat, eat at least 2½ cups of vegetables and fruits each day, and choose whole grains instead of refined-grain products (American Cancer Society 2021b).
Be Physically Active
Women who exercise regularly have 10%-25% lower risk of breast cancer (Eliassen et al. 2010) This benefit is even greater in postmenopausal women (Hildebrand et al. 2013). Avoid sedentary behavior and participate in at least 150 minutes of moderate-intensity (e.g., brisk walking) aerobic exercise, and two days of muscle strengthening exercise per week (USDHHS, 2018).
Get Screened
Early detection and effective treatment have resulted in a 36% decline in breast cancer mortality in the U.S. between 1989 and 2012 (Howlader et al. 2015).
Avoid Drinking Alcohol
Data from 53 studies found that the relative risk of breast cancer increased by about 7% for each alcoholic drink consumed per day. Women who had two to three alcoholic drinks per day had a 20% higher risk of breast cancer (Hamajima et al. 2002).
Breastfeed
Breastfeeding is associated with a slight reduction in a woman’s overall risk of breast cancer. Breastfeeding for a longer duration reduces the risk further (Faupel- Badger et al. 2013)
Remember: Being a woman puts you at risk for breast cancer (fig. 4).

Glossary of Terms
breast lump – Growth of tissue within your breast.
distant stage cancer – Cancer that has spread to organs or tissues in other parts of the body.
estrogen – General term for female steroid sex hormone.
five-year relative survival rate – The proportion of persons surviving five or more years after cancer diagnosis compared with the proportion of survivors expected in a set of comparable cancer-free persons.
localized stage cancer – Cancer that is limited to the tissue or organ in which it started and has not spread to surrounding tissue.
mammogram – Photograph of breasts made by X-rays. mastectomy – Surgical removal of all or part of the breast.
progesterone – General term for male steroid sex hormone.
regional stage cancer – Cancer that has spread beyond the original primary tumor to nearby tissues, organs, or lymph nodes.
Additional Resources
National Cancer Institute: https://www.cancer.gov/.
American Cancer Society: https://www.cancer.org/.
Centers for Disease Control and Prevention: https://www.cdc.gov/cancer/breast/.
Surveillance, Epidemiology, and End Results Program: https://seer.cancer.gov/.
American Institute for Cancer Research: https://www.aicr.org/.
References
American Cancer Society. 2021a. “American Cancer Society Recommendations for the Early Detection of Breast Cancer.” Last revised April 22, 2021. https://www.cancer.org/cancer/breast-cancer/ screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html.
American Cancer Society. 2021b. Cancer Facts and Figures 2021. Atlanta: American Cancer Society. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2021.html.
American Cancer Society. 2019a. “Breast Cancer Signs and Symptoms.” https://www.cancer.org/cancer/ breast-cancer/screening-tests-and-early-detection/ breast-cancer-signs-and-symptoms.html.
American Cancer Society. 2019b. Cancer Treatment and Survivorship: Facts and Figures 2019-2021. Atlanta: American Cancer Society
American Cancer Society. 2019c. “Types of Breast Cancer.” Last revised November 19, 2021. https://www.cancer.org/cancer/breast-cancer/about/ types-of-breast-cancer.html
American Cancer Society. n.d.a “Breast Cancer Early Detection and Diagnosis.” Accessed on August 2, 2021. https://www.cancer.org/cancer/breast-cancer/ screening-tests-and-early-detection.html.
American Cancer Society. n.d.b “Treating Breast Cancer.” https://www.cancer.org/cancer/breast-cancer/treatment.html.
American Cancer Society. n.d.c “Breast Cancer Risk and Prevention: Risk Factors for Breast Cancer” https://www.cancer.org/cancer/breast-cancer/risk-and-prevention.html. Eliassen A. H., G. A. Colditz, B. Rosner, W. C. Willett, and S. E. Hankinson. 2006. “Adult Weight Change and Risk of Postmenopausal Breast Cancer.” Journal of the American Medical Association 296 (2): 193–201. https://doi.org/10.1001/jama.296.2.193.
Eliassen A. H., S. E. Hankinson, B. Rosner, M. D. Holmes, and W. C. Willett. 2010. “Physical Activity and Risk of Breast Cancer among Postmenopausal Women.” Archives of Internal Medicine 170 (19): 1758–64. https://doi.org/10.1001/ archinternmed.2010.363.
Faupel-Badger, J. M., K. F. Arcaro, J. J. Balkam, A. H. Eliassen, F. Hassiotou, C. B. Lebrilla, K. B. Michels, et al. 2013. “Postpartum Remodeling, Lactation, and Breast Cancer Risk: Summary of a National Cancer Institute-Sponsored Workshop.” Journal of the National Cancer Institute 105 (3): 166–74. https://academic.oup.com/jnci/article/105/3/166/1031395
Hamajima N., K. Hirose, K. Tajima, T. Rohan, E. E. Calle, C. W. Heath Jr., R. J. Coates, et al. (Collaborative Group on Hormonal Factors in Breast Cancer). 2002. “Alcohol, Tobacco and Breast Cancer - Collaborative Reanalysis of Individual Data from 53 Epidemiological Studies, Including 58,515 Women with Breast Cancer and 95,067 Women Without the Disease.” British Journal of Cancer 87(11):1234–45. https://doi.org/10.1038/sj.bjc.6600596.
Hildebrand, J. S., S. M. Gapstur, P. T. Campbell, M. M. Gaudet, and A. V. Patel. 2013. “Recreational Physical Activity and Leisure-time Sitting in Relation to Postmenopausal Breast Cancer Risk.” Cancer Epidemiology, Biomarkers and Prevention 22(10):1906-12.
Howlader, N., A. M. Noone, M. Krapcho, J. Garshell, D. Miller, S. F. Altekruse, C. L. Kosary, et al. (eds). 2015. SEER Cancer Statistics Review, 1975-2012, National Cancer Institute. Bethesda, MD. https://seer.cancer.gov/archive/csr/1975_2012/.
Key, T. J., P. N. Appleby, G. K. Reeves, A. W. Roddam, K. J. Helzlsouer, A. J. Alberg, D. E. Rollison et al. (Endogenous Hormones and Breast Cancer Collaborative Group). 2011. “Circulating Sex Hormones and Breast Cancer Risk Factors in Postmenopausal Women: Reanalysis of 13 Studies.” British Journal of Cancer 105:709–22. https://doi.org/10.1038/bjc.2011.254.
National Cancer Institute. 2021a. “Breast Cancer Risk in American Women.” Reviewed December 16, 2020. https://www.cancer.gov/types/breast/risk-fact-sheet.
National Cancer Institute. 2021b. “Breast Cancer Treatment (Adult) (PDQ®)–Patient Version.” Updated October 4, 2021. https://www.cancer.gov/ types/breast/patient/breast-treatment-pdq.
National Cancer Institute. 2014. Understanding Breast Changes: A Health Guide for Women. Downloaded from https://www.cancer.gov/types/breast/breast-changes/understanding-breast-changes.pdf.
National Cancer Institute Surveillance, Epidemiology, and End Results Program. n.d. “Cancer Stat Facts: Female Breast Cancer.” Accessed Aug. 2, 2021. https://seer.cancer.gov/statfacts/html/breast.html.
NCCN (National Comprehensive Cancer Network). 2021. Clinical Practice Guidelines in Oncology. Breast Cancer Screening and Diagnosis. Version 1.2021-May 6, 2021. National Comprehensive Cancer Network. Available for subscribers at https://www.nccn.org/professionals/physician_gls/ pdf/breast-screening.pdf.
U.S. Cancer Statistics Working Group. 2021. “U.S. Cancer Statistics: Data Visualizations.” https://www.cdc.gov/cancer/uscs/dataviz/index.htm.
U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd edition. Washington, DC: U.S. Department of Health and Human Services; 2018.
U.S. Preventive Services Task Force Guidelines. 2016. “Breast Cancer: Screening.” https://www.uspreventiveservicestaskforce.org/ uspstf/recommendation/breast-cancer-screening.
Virginia Cooperative Extension materials are available for public use, reprint, or citation without further permission, provided the use includes credit to the author and to Virginia Cooperative Extension, Virginia Tech, and Virginia State University.
Virginia Cooperative Extension is a partnership of Virginia Tech, Virginia State University, the U.S. Department of Agriculture (USDA), and local governments, and is an equal opportunity employer. For the full non-discrimination statement, please visit ext.vt.edu/accessibility.
Publication Date
June 8, 2022