Understanding the Public Health Risks of Antimicrobial Resistance
ID
HORT-260NP
With the current public uproar about antimicrobial resistance (AMR), it is hard to believe that we understand very little about the main ways antimicrobial resistant bacteria (ARB) can spread to humans. A lot of attention is placed on the food animal industry when it comes to AMR, since the majority of antibiotics by weight in the United States are used for food-producing animals. However, just because antibiotics or ARB may be found in manure or urine after an animal has been treated with antibiotics, does not necessarily indicate a public health threat. There are an extraordinary number of other factors that determine whether those antibiotics or ARB will eventually make their way to humans and, once there, cause an antibiotic resistant infection. While there is much we do know about the public health risks of antimicrobial resistance, there are still many things we do not know.
What We Know
There is no doubt that antimicrobial resistance (AMR) is a global health concern. The Centers for Disease Control and Prevention (CDC) reports that the incidence of antimicrobial resistant infections in people has risen dramatically in recent years. It is estimated that at least 2,049,442 illnesses and 23,000 deaths in the U.S. alone can be attributed to AMR. We know that some bacteria have become more resistant than others and that certain antibiotics have become less effective than others. We also know that antibiotic misuse and overuse has greatly sped up the development of antimicrobial resistance and that the responsible use of antimicrobial drugs is important in every industry.
While we understand that antimicrobial resistance poses a threat to the future effectiveness of life-saving antibiotic drugs, there are many questions still left unanswered, particularly when it comes to the transfer of ARB from animals and the environment to humans.
What We Still Need to Understand
One of the most important things we still need to learn about AMR is the particular hazards and risks of using antibiotic drugs.
A hazard is a potential source of an adverse health effect, whereas a risk is the probability of experiencing an adverse health effect if exposed to a hazard.
Example:
Sarah is walking down the sidewalk. There is a banana peel lying in her path. Considering the width of the path and how closely Sarah is paying attention to where she is walking, she may or may not step on the banana peel, fall, and break her wrist.
What is the hazard in this scenario? The banana peel
What is the risk in this scenario? The probability that Sarah will step on the peel, fall, and break her wrist
In the scenario above, there are countless factors that determine whether or not Sarah will step on the banana. She may notice the banana and step around it, a good Samaritan may point out the banana peel to Sarah before she reaches it or Sarah may actually step on the banana peel but the good grip on her shoes prevents her from falling. These are just a few examples that determine the risk of Sarah getting hurt by stepping on the banana peel. So, what does this mean in terms of antimicrobial resistance?
Hazards, Risks, and Antimicrobial Resistance
Researchers will often report the amount of antibiotics, or ARB that they find in a sample. The sample itself represents a hazard because it is a potential source of a human health threat. Researchers can only use that data and compare it to data from other samples taken to determine if it is “better” or “worse” than other samples. In experiments, these samples are compared to a background value of antibiotics. The background value is the measurement from a sample that was not treated with antibiotics.
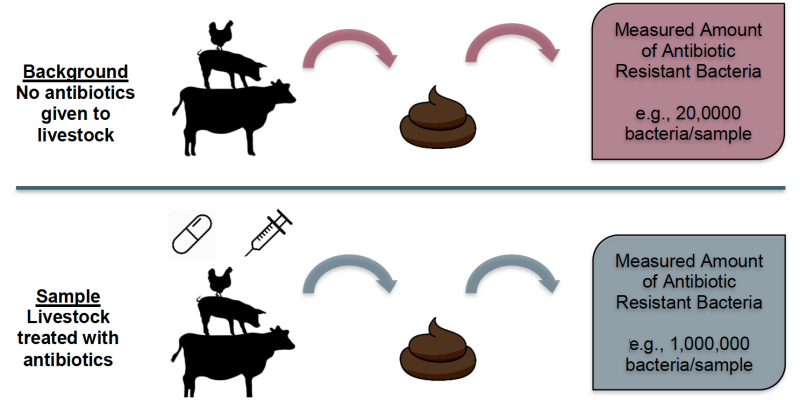
In this example, the background sample contained 20,000 resistant bacteria, and the sample from the animal that was given antibiotics had 1,000,000 resistant bacteria. Therefore, it appears that giving antibiotics to an animal increases the amount of ARB in manure by 980,000, compared to an animal not given antibiotics. The manure represents a hazard because it is a potential source of antibiotic resistant bacteria.
1,000,000 bacteria/sample- antibiotic treated
- 20,000 bacteria/sample- background
980,000 bacteria/sample
In this example, there are 980,000 more bacteria in a sample of manure from an animal given antibiotics than in an animal not given antibiotics.
While we know in this example that manure is a hazard, we cannot calculate what the risk of the antibiotics in the manure is to humans. This is because we do not know the likelihood that someone will contract an antibiotic resistant infection because of the ARB in the manure. For instance, if the manure containing ARB contaminated produce that someone ingested, we do not know how much more likely a person that ingested that produce is to become sick compared to someone that ate uncontaminated produce. The risk may be much higher, or it may be very small. We do not know the risk because, as of 2017, there are no published guidelines telling us what types or concentrations of antibiotics or what kinds or levels of ARB pose a measureable risk to human health.
Why is it so Difficult to Understand the Public Health Risks of AMR?
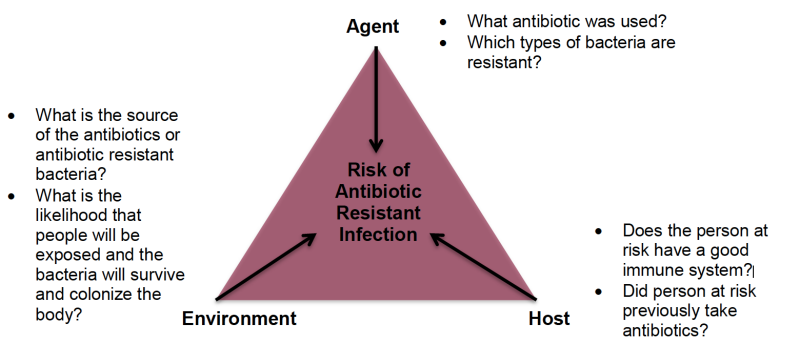
AMR is a very complex phenomenon because of the numerous factors that contribute to it. Some examples of these factors range from the antibiotic type, the type of resistant bacteria, how virulent the bacteria are, the individual qualities of people such as the functionality of their immune system, and the purpose of antibiotic use (e.g., infection, growth, prophylactic). All of these different factors can contribute to the risk of developing an antibiotic resistant infection.
Why do Hazards and Risks Matter?
It is critical to understand both the different hazards and risks associated with antimicrobial use. If we identify the hazards (potential sources of AMR), we will be able to minimize those hazards as much as possible. By identifying the risks associated with the various hazards, we will better understand how to protect the public from the adverse health effects of AMR while maintaining the ability to use antibiotic drugs safely.
AMR affects everyone, from farmers to doctors to patients that need antibiotics for an illness. Antimicrobial drugs save lives, improve welfare, and have economic advantages. Understanding the public health complexities of AMR can help make informed conclusions and decisions when it comes to antimicrobial use and consumption.
References:
CDC information on antimicrobial resistance. Available from: https://www.cdc.gov/drugresistance/about.html. Accessed July 14, 2017.
CDC report on antibiotic resistance threats in People and Animals. Available from:
https://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf#page=25. Accessed July 14, 2017.
Hazard and Risk. Available from: http://www.hsa.ie/eng/Topics/Hazards/. Accessed July 14, 2017.
World Health Organization information on antimicrobial resistance. Available from:
http://www.euro.who.int/en/health-topics/disease-prevention/antimicrobial-resistance/about-amr. Accessed July 14, 2017
Virginia Cooperative Extension materials are available for public use, reprint, or citation without further permission, provided the use includes credit to the author and to Virginia Cooperative Extension, Virginia Tech, and Virginia State University.
Virginia Cooperative Extension is a partnership of Virginia Tech, Virginia State University, the U.S. Department of Agriculture (USDA), and local governments, and is an equal opportunity employer. For the full non-discrimination statement, please visit ext.vt.edu/accessibility.
Publication Date
March 29, 2023